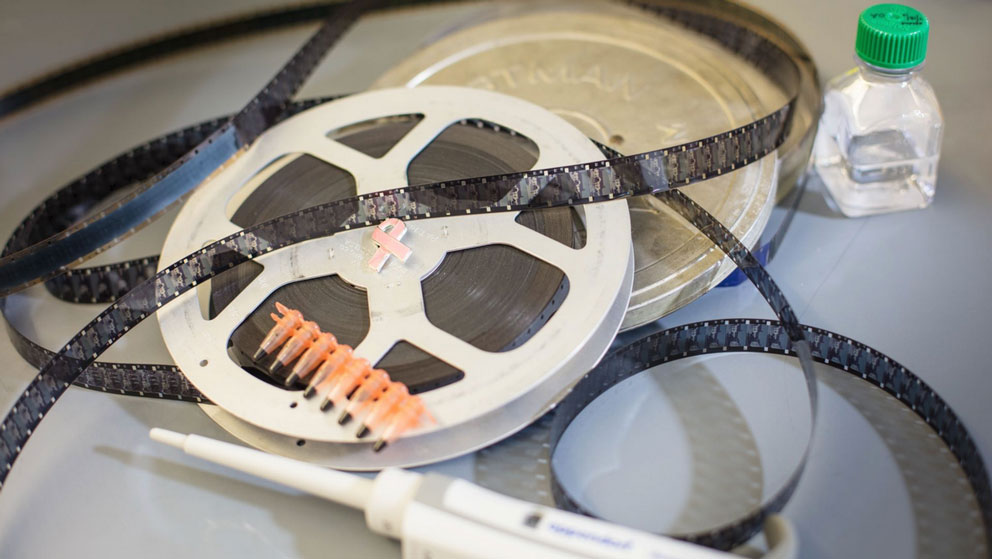
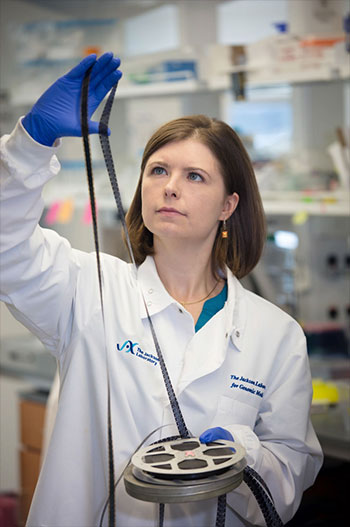
Whether joining together pieces of film or our genes, splicing controls how information is conveyed. Olga Anczuków is exploring this fundamental process to discover new treatments for breast cancer.
Like many creative endeavors, movies contain only a fraction of the footage collected during filming. Indeed, hours of outtakes are removed — left on the cutting room floor — and never make it in to the final product.
Surprisingly, the genome has a cutting room floor, too.
The proteins in our bodies are built from instructions written within our genes. Yet these instructions are interspersed with unusable material — the genomic equivalent of outtakes — and must first be stitched together into a single, uninterrupted thread through a process known as RNA splicing.
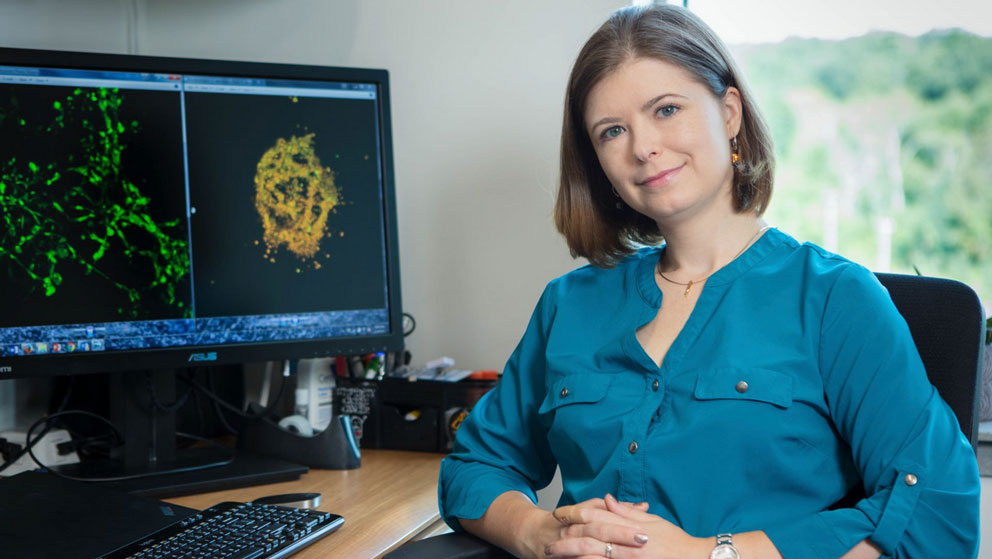
“You can add in or delete a scene and really change the meaning of the movie,” explains Olga Anczuków-Camarda, Ph.D.Investigates how alternative RNA splicing contributes to cancer with the goal of identifying novel clinical biomarkers and targets for precision medicine.Olga Anczuków, Ph.D., an assistant professor at The Jackson Laboratory. “Similarly, with RNA splicing, depending on which parts of a gene are included or excluded, the message can be very different.”
RNA splicing has long been recognized for its fundamental role in biology. But only recently has it generated excitement as a viable therapeutic strategy for a host of diseases, including cancer. Anczuków and her laboratory comprise one of the few teams in the world who are driving progress in this new and important area. “There are a lot of people who work on splicing, and a lot who work on cancer. But there is a need for more people who can combine both disciplines together — I guess that’s what really makes my work unique.”
Elaborate machinery
Despite its critical role in biology, RNA splicing remains poorly understood — especially its contributions to cancer.
“It’s such a critical step in gene expression regulation,” says Anczuków. “We know a lot about it from a mechanistic point of view, but it has been underexplored in the development of normal tissues as well as in diseases.”
Her interest in the area stems from a deep-seated passion for genetics and cancer. Originally from Poland, Anczuków pursued her undergraduate and graduate studies in Lyon, France where she conducted research on molecular genetics and breast cancer at the International Agency for Research on Cancer (part of the World Health Organization) and later at the School of Medicine and University Claude Bernard Lyon 1. As a graduate student, she delved into the molecular causes of breast cancer, studying different mutations in the BRCA1 and BRCA2 genes, which can predispose women who carry them to breast and ovarian cancer.
“We uncovered some mutations that affect RNA stability and others that affect RNA splicing, “ says Anczuków. “That’s really what got me interested in RNA splicing as a mechanism of tumor progression.”
The molecular machinery responsible for RNA splicing is as elaborate as it is impressive. Hundreds of different components come together to snip out the unwanted segments of genes (called “introns”) and join together the desirable parts (called “exons”), all before proteins can be made. Typically, small genes harbor somewhere between five and ten introns that need to be removed. Large genes have many more. In addition, exons can be strung together in different combinations, like a set of Legos assembled into varying shapes. This process, known as alternative splicing, enables a single gene to create multiple different proteins — scores of them, in some cases — each with different functions. Some forms of a protein may push cells to proliferate, others may coax the cells to stop growing or even to die.
“It provides a very efficient way of fine-tuning the expression of genes, so it’s probably not surprising that it gets disrupted in cancer,” she says.
Looking beyond DNA
To understand how and why splicing runs amok in cancer, Anczuków and her colleagues are sifting through mountains of data collected from patients’ tumors — especially triple-negative breast tumors, which are notoriously difficult to treat. Bolstered by large-scale projects like The Cancer Genome Atlas and powerful genomic technologies for decoding tumors’ RNA and DNA, the scientists can conduct a kind of molecular census of the splicing machinery, determining which components are present or not, as well as their relative abundances. Anczuków and her team are not searching for mutations in the splicing factors genes per se, but instead for evidence that these factors are present at abnormally high levels — and therefore much more active than they should be.
“We’re looking beyond DNA, beyond the classical mutations, and trying to figure out how we can use the information embedded within splicing machinery to predict which patients’ tumors are likely to metastasize or which ones are likely to respond to a certain kind of therapy,” says Anczuków.
Her laboratory is also on the hunt for novel cancer therapies that can shrink a tumor or stop if from spreading. Once they uncover molecular evidence of aberrant splicing in human tumors, they move on to validate their findings using a variety of experimental systems.
“If we want to increase our likelihood of finding novel drugs and therapies, we really need to choose the right model systems,” she says. For Anczuków, that means a combination of approaches, including three-dimensional cultures of human mammary cells. These breast cells are grown in a Jell-O-like matrix, giving them the support they need to form three-dimensional structures, including ducts — nearly identical to those found in the body.
In addition to these breast “organoids,” Anczuków and her colleagues also leverage various mouse models, including those that carry human tumors (so-called PDX mice), which enable the researchers to propagate and study cancer cells that more closely resemble those found in patients. It turns out that growing tumor cells in a tiny plastic dish — a convenient, time-honored method followed in many laboratories — can fundamentally alter cancer cells’ biology, essentially rewiring them for life in an artificial environment instead of the human body. And that rewiring is not necessarily an accurate reflection of their original, cancer-causing state. JAX boasts a wealth of expertise in a variety of mouse cancer models, which is helping to propel Anczuków’s research.
“One of the things that drew me to JAX is the ability to benefit from such extraordinary expertise through collaborations with my colleagues here,” she says.
Anczuków is also striking up collaborations with colleagues at other institutions, including nearby UConn Health. She recently began working with Brent Graveley, professor and interim chair of genetics and genome sciences at UConn Health and a renowned expert in RNA splicing. The two have traveled in the same professional circles for years, but only now have they had an opportunity to work together.
“I was quite impressed with her research,” says Graveley. “She’s very enthusiastic and full of energy. When I found out she was a candidate for a position at JAX, I was very excited.”
Since Anczuków arrived at JAX just over a year ago, she and Graveley have mapped out their projects and are now beginning to launch them. Although the work is in its infancy, the two scientists bring distinct — and quite complementary — skills to the table. Graveley studies the biochemical mechanisms of RNA splicing, delving into the mechanisms that underlie the process in normal cells, while Anczuków’s expertise lies in the biological outcomes of aberrant splicing and their impact on cancer biology.
“It’s very early days, but I think there is tremendous promise,” says Graveley. “For almost every disease out there, somewhere between 15 and 20 percent of all mutations that cause that particular disease have some impact on splicing. The more we understand how splicing works and how it is regulated, the more we will be able to come up with strategies for targeting splicing in a broad spectrum of disorders.”
A new drug based on RNA splicing research
Late last year, a revolutionary new drug gained approval by the Food and Drug Administration. Known as Spinraza™ (generic name nusinersen), the drug targets the RNA splicing machinery to enable the production of a key protein called SMN (short for survival of motor neurons). As its name implies, the protein is required for the formation and survival of motor neurons; without it, the cells die, causing a severe and sometimes fatal genetic condition known as spinal muscular atrophy (SMA).
One of the earliest architects of this remarkable new drug was Adrian Krainer of Cold Spring Harbor Laboratory, a pioneer in the field of RNA splicing and Anczuków’s postdoc mentor.
“This approach, which harnesses chemical technology to deliver a therapeutic made out of RNA, really opens the possibility of targeting virtually any RNA molecule in our cells — even things that cannot be targeted through more conventional means, such as antibodies or small molecules,” she explains. Although it has so far been applied only to SMA — a disease in which only one gene is affected, compared to cancer, where many genes are impacted — Anczuków is enthusiastic about its potential in breast and other cancers.
“I think targeting splicing is a very exciting therapeutic strategy now for many people in the cancer field,” she says. “I am confident that we will develop a new drug that targets RNA splicing in breast cancer.”
Nicole Davis, Ph.D., is a freelance writer and communications consultant specializing in biomedicine and biotechnology. She has worked as a science communications professional for over a decade and earned her Ph.D. studying genetics at Harvard University.