 Cultural competency is defined as the ability to understand, appreciate and interact with people from a culture or belief systems different from one’s own (American Psychological Society 2015). Healthcare providers who can employ cultural competence help eliminate disparities in care.
Cultural competency is defined as the ability to understand, appreciate and interact with people from a culture or belief systems different from one’s own (American Psychological Society 2015). Healthcare providers who can employ cultural competence help eliminate disparities in care.
We’ve known for a long time that being “culturally sensitive” is not enough. Twenty-five years ago, Lavizzo-Mourey & Mackenzie (1996) made the case that to achieve cultural competence and understand how diversity affects patient outcomes, clinicians need to incorporate three population-specific issues: (1) health-related beliefs and cultural values, (2) disease incidence and prevalence, and (3) treatment efficacy. As an example, a patient’s traditional beliefs may differ from mainstream medical care, such that they may view receiving genetic results and making medical decisions based on that information as a family affair. Other cultures hold the belief that language can shape reality, so that receiving news about disease risk framed in a negative way can be upsetting. Disregarding cultural factors may add stress to an already difficult situation, impacting mental health, quality of life and negative health behaviors.
Clinical Education at JAX wants to acknowledge that we are not experts in achieving cultural competence, but we want to help our learners recognize how diversity, equity, and inclusion apply in the provision of genetic care or in assessing for referral to genetics.
Implementing changes with a sense of cultural humility is key. Healthcare professionals can improve their awareness of implicit biases and foster an approach to patients characterized by openness and curiosity about each new patient through ongoing exploration of and reflecting on their own beliefs and behaviors (Georgetown University Health Policy Institute).
Five things to increase cultural competence in genetic medicine
Recent discussions in healthcare, and throughout society, raise awareness about how people identify and how the intersectionality of identities makes each of us who we are. Practicing with cultural competence respects and embraces the multitude of identities that comprise diversity. Below we have outlined what this may mean for your practice, with a focus on where it may intersect with genetics. These discussions include:
1. Creating a welcoming environment for all
Have you ever had an unexpected reaction from a patient? Perhaps they felt unwelcome in some way. There are small ways to change the set up of your practice and the language staff uses to foster a welcoming environment, such as for your LGBTQ+ patients.
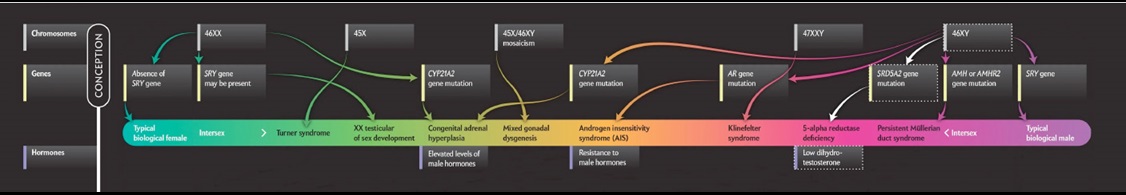
Be aware that gender is not binary. Genetic medicine and sex differentiation are closely entwined, creating a complex web of genetics, anatomy, physical sexual characteristics, and gender identity. (For an idea of how incredibly complex this is, take some time to review this admittedly complicated resource, adapted from Scientific American.)
Maybe you’ve had a patient you were unsure how to address, or you made an assumption and were wrong. By adding your pronouns to your nametags, and consistently introducing yourself with the pronouns you use, followed by a genuine inquiry about the pronouns the patient uses, you will signify that your practice is welcoming to all. “Using pronouns, even if you are cis-gendered, normalizes the use of pronouns and makes it easier for our nonbinary and trans community members to do the same.” (DasGupta 2021).
If you work in an ob/gyn or prenatal setting, simple changes in language can go a long way. Use “sex of the baby” rather than “gender,” avoid binary terms such as “boy or girl,” use “parents” instead of “Mom and Dad.”
In an oncology setting, de-gender language about organs. Instead of “female reproductive cancers” name the specific organs. Likewise for hormones, name them specifically rather than using “male and female hormones.”
When genetic assessment involves intellectual or physical disability, remember the patient (or relative) is living with that disability. Your language can reflect a wholistic approach to the person, using language such as a “son with autism” rather than an “autistic son.”
Of course, not everyone is comfortable with the same terms, and some embrace their disability as part of their identity (e.g., I am a disabled person not someone living with a disability). Follow your patient’s lead or ask their preference if unsure. This demonstrates respect for patient autonomy and builds trust. Establishing respect and trust will lay a foundation for a safe space to examine the range of emotions genetic testing may elicit.
2. Collecting personal and family history information equitably
People in historically underrepresented populations face barriers in genetic assessment (Chapman-Davis 2021, Cragun 2017, Cragun 2019, Schaa 2015) in part because providers are less likely to evaluate their family medical history and less likely to recommend genetic counseling/testing when appropriate. Notice if you are asking family history questions differently or making assumptions about family dynamics when assessing underrepresented minority patients for a genetics referral. Sensitive family history collection questions include inquiring about diagnoses in estranged relatives, gender identity or sex assigned at birth. Preface these with the reason why you are asking. A woman may be estranged from her father, but with an explanation that inherited cancer risk can come from the paternal side of the family as well as the maternal side, she may be more comfortable talking about that side of her family when she understands it may impact your risk assessment or decision about referring to genetic services.
Address privacy concerns, such as who may have access to the pedigree. Transgender patients may not wish for other healthcare providers to know. If you use pedigrees to note family history information, look to the National Society of Genetic Counselors for articles and updated practice guidelines on notating transgender and non-binary gender identity in pedigrees.
Family history collection often includes a discussion of the patient’s diagnosis. Open discussion about a diagnosis may be very uncomfortable in some cultures. To elucidate whether your patient is at ease with discussing their diagnosis, prioritize rapport over comprehensive information. Ask: “Is this relevant to you? Would you like to hear more about this?” When asking sensitive questions, explain openly why you are asking so you can build trust.
Low health, numeric and genomic literacy may also be a barrier to communicating genetic risk. More than one-third of Americans have basic or below basic health literacy. Communicating effectively can make a difference in whether your patient accepts a referral to genetic services or decides to proceed with genetic testing. Conveying too much genetic information can be counterproductive. Instead use plain language without genetic jargon: runs in the family vs. hereditary, close/distant relative vs. first-/third-degree relative, higher chance vs. predisposition. Focus on take home messages, balancing what may be your wish to communicate accurately with achieving clarity. Consider using a teach-back method to ensure patient understanding. Try saying you’d like to make sure you did a good job explaining this information and ask them to tell you what they would share with family members or their partner. See the National Genetics Education and Family Support Center’s All About Genetics plain language resources, the AHRQ’s Health Literacy Universal Precautions Toolkit, and JAX’s Communicating Genetic Risk resource for tips on discussing numeric information with patients.
3. Using interpreter services effectively
Discussing genetic information, reasons for a referral and pre- and post- test counseling are complex. Relying on English speaking family members can create conflict and even upset the social norms of your patient’s culture. Most language interpreters are trained in basic health language but not genetics specifically. Consider implementing training; the National Coordinating Center for Regional Genetics Networks provides a curriculum for interpreters in medical genetics. And keep on the lookout for language-specific resources such as these from the Minority Genetic Professionals Network.
4. Continuing implicit bias training
Participate in system-wide training at your institution, and apply the lessons learned to genomic care in your practice. We all hold unconscious biases, even as healthcare providers.
Disability, as an example, is prevalent in the general population and many genetic diagnoses include physical or intellectual disabilities. Highlighting the importance of continued training are recent studies of disability bias in the prenatal setting from Project Inclusive, which demonstrated explicit and implicit disability bias among providers. Interventions were effective in decreasing bias in recommendations regarding genetic testing and pregnancy termination. Professional experience with individuals with disabilities, training in patient-centered counseling and self-reflection about disability bias were all effective. While the researchers concluded that these findings can be applied to training programs, practicing clinicians can seek out these opportunities as well.
5. Supporting efforts to increase diversity in the genomic workforce
Longer term, recruiting team members with a variety of backgrounds and identities will improve inclusiveness in the provision of genetic services. For example, in October, 2021, the National Human Genome Research Institute (NHGRI) formed a new Office of Training, Diversity and Health Equity to further the development of a more diverse genomic workforce to address disparities.
How will this help the patients referred to genetic services? Deepti Babu, a genetic counselor and chair of the National Society of Genetic Counselors’ JEDI Committee, says “Diversifying our workforce allows us to better represent and understand all patients and communities we serve. With this understanding, we can find new ways to help everyone that needs access to genetics care.” This can be accomplished by forging relationships with schools, starting earlier to foster interest in STEM careers and engaging with historically Black colleges and universities (HBCUs).
Spread the word about the Minority Genetic Professionals Network. The MGPN uses a framework of education, mentoring and support to help minority students learn about professions in genetics. Even if you do not provide genetic services yourself, sharing this resource with students you know can help diversify the genomics workforce for the future.
Increasing cultural competence in genomic care will not happen overnight. We encourage you, your team, and your organization to commit to making changes in your practice. Meanwhile, if you make a mistake? Lean on cultural humility with a short, sincere apology and move on.
Want to share what has worked in your practice? Tweet us at @JAXClinicalEd.
References
- Babu, D. [@GeneticCouns]. (2021, Sept 30). Diversifying our workforce allows us to better represent and understand all patients and communities we serve. With this understanding, we can find new ways to help everyone that needs access to genetics care. [Tweet]. Twitter.
- Chapman-Davis E, et al. Racial and Ethnic Disparities in Genetic Testing at a Hereditary Breast and Ovarian Cancer Center. J Gen Intern Med. 2021 Jan;36(1):35-42.
- Cragun D, et al. Racial disparities in BRCA testing and cancer risk management across a population-based sample of young breast cancer survivors. Cancer. 2017;123(13):2497-2505.
- Cragun D, et al. Genetic Testing Across Young Hispanic and Non-Hispanic White Breast Cancer Survivors: Facilitators, Barriers, and Awareness of the Genetic Information Nondiscrimination Act. Genet Test Mol Biomarkers. 2019 Feb;23(2):75-83.
- DasGupta, S. [@prof_dasgupta]. (2021, Sept 30). Using pronouns, even if you are cis-gendered, normalizes the use of pronouns and makes it easier for our nonbinary and trans community members to do the same [Tweet]. Twitter.
- Lavizzo-Mourey RJ, MacKenzie E. Cultural competence--an essential hybrid for delivering high quality care in the 1990's and beyond. Trans Am Clin Climatol Assoc. 1996;107:226-35; discussion 236-7.
- Midwest Genetics Network. [@Region4Geentics]. (2021, September 30) https://twitter.com/hashtag/MGNTweetChat?src=hashtag_click
Schaa KL, et al. Genetic counselors' implicit racial attitudes and their relationship to communication. Health Psychol. 2015 Feb;34(2):111-9.