Uncovering the mechanisms of phage transfer between bacteria
Research Highlight | April 14, 2017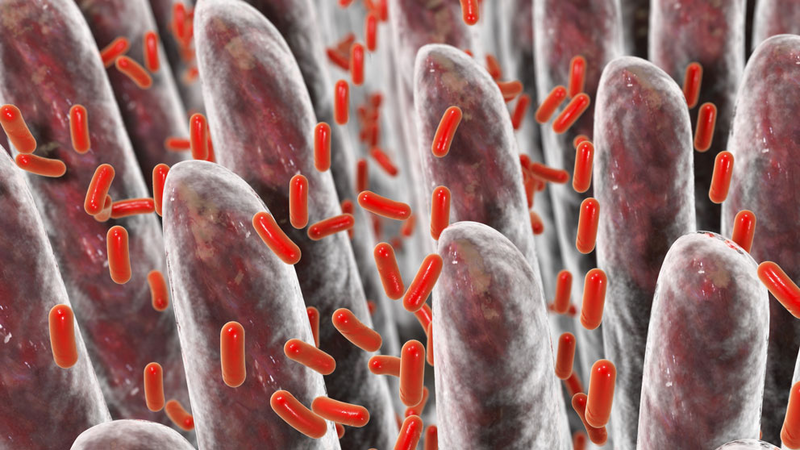
Bacteria swap viruses during intestinal infection in the mouse
Our genome is not exclusively our own. Humans are silently (latently) infected with many viruses that insert themselves into our DNA. Common examples include cytomegalovirus, Epstein-Barr virus, and BK virus. Most of our latent viral partners do not cause us harm, and some only become harmful when our health balance is shifted, such as when we contract another serious infection (i.e., HIV), or have a chronic illness (i.e., type II diabetes), or have an organ transplant. In these cases, the viruses that were peacefully squatting in our genome begin to replicate themselves, causing infection and all the pathology associated with it.
Viruses can latently infect bacteria too; these are called prophages, or just phages for short. Similar to latent human viruses, prophages are mostly benign. But if the infected bacterium is stressed, the virus can reactivate; it will pop out of the bacterial genome, replicate, and go on to infect other bacteria and insert itself into a new genomic host.
Although it sounds bad (kind of like catching a cold), there can be benefits to the bacterium contracting the new virus. Often, phages also contain some bacterially derived DNA from the originating cell, and this foreign DNA can be incorporated along with the viral genome, giving the newly infected bacteria more genes to play with. This is one mechanism by which bacteria swap genes between one another — like antibiotic resistance genes — and the main reason why phage transfer between bacteria is medically relevant. If scientists understood how and why phages hop from one bacterial strain to another, we could find new ways to stem the spread of antibiotic resistance genes and prolong the usefulness of existing antibiotic drugs.
Microbiologists have been studying phage transfer between bacteria in the lab for many decades, but less was known about how phages hop from one bacterium to another within a host organism. To get at this mechanism, Médéric Diard and colleagues used some fancy genetic tools and tried-and-true mouse models to figure out howSalmonella swap viruses during an intestinal infection. The findings were published in a recent report in Science.
Salmonella is a common bacterial source of food-borne illness. You may remember Salmonella from the contaminated peanut butter outbreak of 2008-2009 that killed nine people and critically sickened more than 700 others across 47 states. In mice, certain strains of Salmonella cause intestinal inflammation and diarrhea, similar to humans, and thus mice are a faithful model for many Salmonella-related infectious and pathological processes.
Diard and colleagues discovered that if they fed mice prophage-containingSalmonella, and then followed up with equal amounts of Salmonella lacking that virus, more than half of the previously uninfected Salmonella strain would now harbor the phage — as recovered from the stool — after only three days of infection. This suggests that the prophage was being activated in gut and passing from one strain to the other. Under laboratory conditions, prophages are commonly activated by bacterial stress responses. Previous research demonstrated that Salmonella induces antimicrobial peptide secretion and recruits granulocytes into the gut of mice, which kills a substantial amount of the infecting bacterial cells. Therefore, since Salmonella infection causes inflammation in the gut, the authors reasoned that the host inflammatory response may be the stress trigger causing prophage activation.
They tested this hypothesis in three ways:
- They knocked out the major stress sensor in the phage-containing bacterium;
- they knocked out the bacterial genes responsible for inducing gut inflammation; and
- they vaccinated the mice against Salmonella to eliminate the inflammatory response when challenged with live bacteria.
In all cases, prophage transfer to the naïve strain was either undetectable or significantly reduced after three days of infection with both bacteria.
Therefore, while the host inflammatory response is critical for the clearance of aSalmonella infection under normal conditions, it actually boosts phage transfer and genetic evolution of the bacteria targeted for destruction. This should be taken into account when considering the benefits of vaccinating livestock and farm animals, which represent common reservoirs of Salmonella and other intestinal pathogen contamination in the human food supply.
