Precision Medicine Meets Immunotherapy
Last week, leaders from multinational pharmaceutical and biotechnology companies, major academic cancer centers, health insurance companies, and other key players, announced the launch of Cancer Moonshot 2020. The program’s sole purpose: accelerating the potential of combination immunotherapies as the next generation standard of care in patients with cancer. (Read our discussion on what makes cancer so difficult to cure.)
While there is nothing new about yet another effort to eradicate cancer, what makes Moonshot 2020 revolutionary is that key players–including the private sector giants Amgen, Celgene, Merck, Glaxo Smith Kline, and spearheaded by NantWorks–are committed to collaborative research efforts, including volunteering collections of new molecules. The consortium aims to accelerate the process of figuring out the best combination of therapies to treat up to 20 tumor types. The ultimate goal is Phase III clinical trials of a cancer vaccine and, by 2020, the “moonshot”—a cancer cure.
R&D divisions at institutions often specialize in developing different classes of cancer therapeutics. While some groups target cancer cells that carry specific mutations using cancer-specific antibodies and vaccines, others focus on developing immuno-stimulant cytokines, engineered NK cells, enriched T cells, or immune checkpoint inhibitors. Although pharma and biotech companies are developing exciting compounds, the chances of success are much greater if these compounds can act together to activate the immune system to detect and destroy cancer cells. By pooling resources, this visionary program will design and conduct dozens of clinical trials using over 60 novel agents, based on the personalized genetic sequencing of 20,000 cancer patients.
Personalized genomics vs. traditional cancer care
Most traditional treatments are tested on broad populations and are prescribed using statistical averages. Consequently, they work for some patients but not for many others, due to genetic differences among the population. On average, a given prescription drug on the market only works for half of those who take it. This traditional practice often fails because each person’s genetic makeup is slightly different from everyone else’s, often in very important ways that affect health and the outcome of cancer treatments.
Personalized medicine involves treating a patient with specific drugs based on her unique genome sequence. This approach is beginning to overcome the limitations of traditional medicine. Tailoring health care to each person’s unique genetic makeup–that is the promising idea behind personalized medicine, also known as individualized medicine, precision medicine, or genomic medicine.
Recently, a consortium of international researchers, including Charles Lee, Ph.D., Professor and Scientific Director at The Jackson Laboratory for Genomic Medicine, sequenced over 2,500 human genomes across the globe and found that a “typical” genome differs from the reference human genome—derived from the Human Genome Sequencing Project—at between 4.1 million and 5.0 million sites. This further emphasizes the fundamental flaw of the one drug-fits-all patients approach and stresses the need to treat cancer patients according to their unique genomic sequence.

Immunotherapies
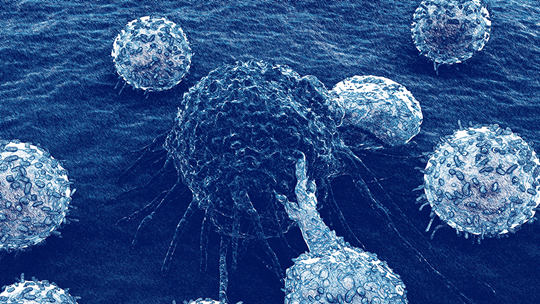
Traditional cancer chemotherapy treatments have many side effects since they indiscriminately kill both cancerous and normal cells. One way to increase specificity and reduce off-target effects is through immunotherapy. Researchers are better understanding the interactions between immune effector cells and tumors, helping discover new ways to boost the body’s immune system to attack cancer cells.
Cancer immunotherapies are treatments that use certain components of the patient’s immune system to detect and eliminate tumor cells. These approaches include treatments that work by different mechanisms. Some boost the body’s immune system in a very general way, while others help train the immune system to attack cancer cells specifically.
As many therapies fail to demonstrate durable remission, the Moonshot 2020 approach will use a personalized combination of immunotherapies and targeted therapies to achieve long-lasting remission. The Quantitative Integrative Lifelong Trial program launched last week is designed to harness and orchestrate all the elements of the immune system, including dendritic cells, T cells, and NK cell therapies.
Moonshot 2020 patients will undergo next generation whole genome sequencing, transcriptome analysis, and quantitative proteomic analysis to participate in customized combinations of the following types of immunotherapeutics:
1. Cancer vaccines
Vaccines, whether designed to target measles, HIV, or cancer, all share the same fundamental principle—to boost the immune system's activity so that it can seek out and destroy the necessary intruder. Cellular targets can include tumor cells and tumor vasculature.
2. Cell-based immunotherapy
The most common cell-based approaches stimulate the patient’s immune system to recognize or kill cancer cells more effectively. Knowledge on the expression of tumor-specific antigens has accumulated such that tumor antigen peptides may be used to prime antigen presenting cells, such as dendritic cells, to stimulate adaptive immune responses before autologous, cancer-killing lymphocytes are reinfused in the patient. See a summary of the different types of cell-based immunotherapies.
3. Metronomic chemotherapy
Toxic effects and chemo-resistance are major obstacles in traditional chemotherapy. “Metronomic chemotherapy” was designed to avoid these problems by administrating chemotherapeutic agents at very low doses (1/10th – 1/3rd of the maximum tolerated dose) but with greater frequency than standard of care chemotherapy.
4. Low dose radiotherapy
In low dose radiotherapy, cancer cells receive continuous low dose radiation from the source over a period of several days or weeks depending on the type of cancer. Typically, patients who receive the low dose schedule have a significant reduction of side effects, while the cancer recurrence rate is similar to patients using standard high-dose schedules
5. Immuno-modulators
Although immune cells are tasked to detect and destroy cancer cells, more often than not, cancer cells are able to inhibit this process. Two immunosuppressive pathways have been implicated in inhibition of tumor infiltrating lymphocytes mediated by cytotoxic T lymphocyte antigen 4 (CTLA-4) and programmed death 1 (PD-1). These are known as “check-point” pathways because they are important in preventing the loss of immune tolerance under normal conditions. These checkpoints can be manipulated with human monoclonal antibodies, such as Ipilimumab, Prembrolizumab, and Nivolumab, to enhance cytotoxic T cell-mediated tumor destruction.
Understanding the interactions between human immune cells and tumors is paramount when devising treatment strategies that prevent tumor evasion of immune cells and improve cytotoxic responses. Tumor-bearing, humanized NSGTM mice are a new valuable preclinical testing platform for immuno-oncology, allowing scientists to gain a better biological understanding of how human immune and tumor cells interact, and enable preclinical testing of new therapies that have a higher likelihood for success when translated to clinical application.
Although details are yet to come, both private and the public elements of the program share the same philosophy: personal genetic sequencing combined with next-generation therapies will enable more effective, customized cancer treatments.